Chronic Osteomyelitis - interesting
Chronic recurrent multifocal osteomyelitis CRMO is an immune-mediated chronic inflammatory self- limiting disease with non-suppurative inflammation involving one or multiple bone foci. A bacterial etiology has not yet been proven, but the investigators hypothesize that CRMO is caused by chronic infection. Using existing knowledge of chronic infections combined with sensitive molecular techniques, the hope is to elucidate the cause of CRMO by proving or disproving bacteria as the underlying etiology. Epidemiology, clinical manifestations and prognosis Chronic recurrent multifocal osteomyelitis CRMO is an immune-mediated chronic inflammatory self- limiting disease with non-suppurative inflammation involving one or multiple bone foci. The disease occurs primarily in children and adolescents.Question: Chronic Osteomyelitis
| My Philosophy Of Teacher Leadership | 442 |
| Chronic Osteomyelitis | James K Polk And Manifest Destiny |
| ADOLESCENT PREGNANCY RISKS OF MOTHER AND HER | 953 |
| The Helmet Of A Motorcycle Car | 275 |
| California Is The Highest Amount Of Electoral | Jan 28, · Chronic recurrent multifocal osteomyelitis (CRMO) is an immune-mediated chronic inflammatory self- limiting disease with non-suppurative inflammation involving one or multiple bone foci. A bacterial etiology has not yet been proven, but the investigators hypothesize that CRMO is caused by chronic infection. 2 days ago · Carcinogenesis and precancerosis transformation of chronic osteomyelitis: 6 cases report and literature review. 1 day ago · Osteomyelitis is an inflammation of bone marrow with a tendency for progression, involving the cortical plates and often periosteal tissues, with most cases occurring after trauma to bone or bone surgery or secondary to vascular insufficiency. |
![[BKEYWORD-0-3] Chronic Osteomyelitis](http://www.imagingpathways.health.wa.gov.au/./images/osteomyelitis/mri_osteomyelitis.jpg) Chronic Osteomyelitis
Chronic Osteomyelitis
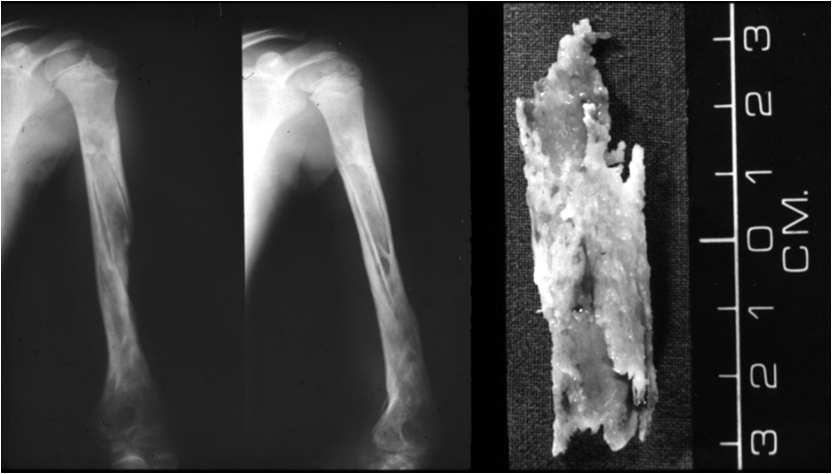
Osteomyelitis is an inflammation of bone marrow with a tendency for progression, involving the cortical plates and often periosteal tissues, with most cases occurring after trauma to bone or bone surgery or secondary to vascular insufficiency.
How to participate?
Despite surgical and chemotherapeutic advancements, osteomyelitis remains difficult to treat, and no universally accepted protocol for treatment exists. Osteomyelitis is also encountered more commonly in tooth-bearing areas and, prior to the advent of antibiotics, osteomyelitis of the mandible was not an uncommon occurrence. With the use of antibiotics, however, osteomyelitis has now become a rare disease. Osteomyelitis of the mandible is much more common than of the maxilla due to its dense and poorly vascularized cortical plates along with the https://amazonia.fiocruz.br/scdp/essay/is-lafayette-a-hidden-ivy/sex-differences-and-aggression-what-are-the.php originating from the inferior alveolar Chronic Osteomyelitis bundle.

Maxillary bone, meanwhile, is much less dense and receives its vasculature from multiple vessels and thus more resistant to developing an osteomyelitis. Host defenses also play a role in the progression of osteomyelitis. Osteomyelitis has been associated with systemic diseases, such as diabetes mellitus, autoimmune disorders, malignancy, malnutrition, and AIDS.
Additional factors that predispose patients to osteomyelitis of the jaws include noncompliant patients who are refractory to health care delivery, patient age, nutritional status, immunosuppression, microvascular disease, and inaccessibility to health care. Medications with roles in osteomyelitis include steroids, chemotherapeutic agents, and bisphosphonates. Local factors that compromise vascularity, such as osteoporosis, bone pathology, and radiation therapy, also increase the possible risk for bony infection. Osteomyelitis typically occurs as a result of spread of an odontogenic infection or as a result of trauma. Chronic Osteomyelitis presence of teeth provides Chronic Osteomyelitis direct pathway to the bone by pulpal or periodontal disease.
Chronic Osteomyelitis
A hematogenous origin is rare and primarily occurs in young children. The adult process begins with bacteria spreading to the jaw bones, either through extraction of Chronic Osteomyelitis, root canal therapy, or fracture of the jaw bones, resulting in a bacteria-induced inflammatory process.
Key points
Although commonly self-limiting, there is a potential for progression to a pathologic process. Inflammation leads to hyperemia, increased blood flow, and leukocytes to the affected area.

When the pus and inflammatory response occur in the bone marrow, elevated intramedullary pressure is created, which further decreases blood flow to jaw bones. Pus travels via the haversian system and Volkmann canals to spread throughout the medullary and cortical bones, and, as pus perforates the cortical bone, it collects under the periosteum, further compromising the periosteal blood Chronic Osteomyelitis. After some time, ultimately the purulence exits the soft tissues via intraoral or extraoral fistulas.
Pathogenesis
Many classification systems for osteomyelitis have been presented in the past, such as suppurative Chronic Osteomyelitis nonsuppurative, hematogenous Chrpnic secondary to a contiguous focus of infection, and acute or chronic, with the latter becoming the predominant Chronic Osteomyelitis system. Another classification system is based on Zurich, in which chronic osteomyelitis can be divided into suppurative chronic osteomyelitis, osteonecrosis of the jaw, and bisphosphonate-related osteonecrosis of the jaw BRONJ. Osteomyelitis may be classified into acute and chronic forms. Acute osteomyelitis can be further subdivided into suppurative and nonsuppurative forms as well as progressive or hematogenous forms. Chronic osteomyelitis may be classified by the causative agent or as suppurative or nonsuppurative forms or sclerosing with subclassifications of diffuse or focal disease.]
One thought on “Chronic Osteomyelitis”